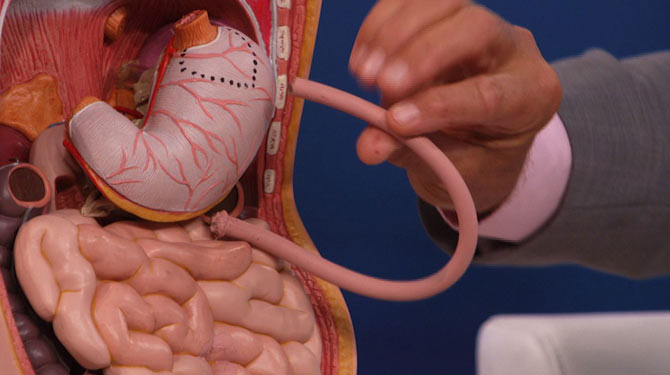
Bariatric surgery (or weight loss surgery) includes a variety of procedures performed on people who are obese. Long term weight loss through standard of care procedures (Roux en-Y bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch) is largely achieved by altering gut hormone levels that are responsible for hunger and satiety, leading to a new hormonal weight set point.
Bariatric surgery is a hormonal surgery in these procedures, for which the alteration in gut hormones develops as a result of the procedure’s restriction and malabsorption.Surgery should be considered as a treatment option for patients with a BMI of 40 kg/m2 or greater who instituted but failed an adequate exercise and diet program (with or without adjunctive drug therapy) and who present with obesity-related comorbid conditions, such as hypertension, impaired glucose tolerance, diabetes mellitus, hyperlipidemia, and obstructive sleep apnea.
A doctor–patient discussion of surgical options should include the long-term side effects, such as a possible need for reoperation, gallbladder disease, and malabsorption. Patients should be referred to high-volume centers with surgeons experienced in bariatric surgery. In the short term, weight loss from bariatric surgeries is associated with reductions in some comorbidities of obesity, such as diabetes, metabolic syndrome and sleep apnea, but the benefit for hypertension is uncertain.
Given the remarkable rate of diabetes remission with bariatric surgery, there is considerable interest in offering this intervention to people with type 2 diabetes who have a lower BMI than is generally required for bariatric surgery, but high quality evidence is lacking and optimal timing of the procedure is uncertain.








