A continuous glucose monitor (CGM) is a device used for monitoring blood glucose on a continual basis by insulin-requiring people with diabetes, e.g. people with type I, type II diabetes or other types of diabetes (e.g. gestational diabetes).
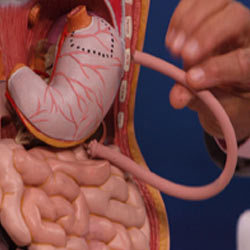
A continuous glucose monitor consists of three parts: a small electrode placed under the skin, a transmitter sending readings at regular intervals (ranging from every 5 to 15 min), and a separate receiver. Currently approved CGMs use an enzymatic technology which reacts with glucose molecules in the interstitial fluid generating an electric current. This electric current (proportional to the glucose concentration) is then relayed from a transmitter attached to the sensor out to a reader which displays the data to the patient.

CGM is an increasingly adopted technology which has shown to have benefits for people with diabetes. Some studies have demonstrated reduced time spent in hypoglycemia or a lower glycated hemoglobin, both favorable outcomes. However, there are important limitations: CGM systems are not sufficiently accurate for detecting hypoglycemia, a common side-effect of diabetes treatment.
This is especially problematic as some devices offer alarm functions to warn of hypoglycemic episodes and people might rely on those alarms. Therefore some manufacturers warn users of relying only on CGM-measurements and the National Institute for Health and Care Excellence recommends to validate hypoglycaemic values via fingerprick testing of blood glucose level.
Another limitation is that glucose levels are taken from the interstitial fluid rather than the blood. As it takes time for glucose to travel from the bloodstream into the interstitial fluid, there is an inherent lag behind the current blood glucose level and the level measured by the CGM. This lag time varies based on the person and the device, and is generally 5–20 minutes.